Distribution of critical care physician workforce in North Carolina
By Heather Wilson, Julie Spero, Dan Jonas, Erin Fraher
May 21, 2020
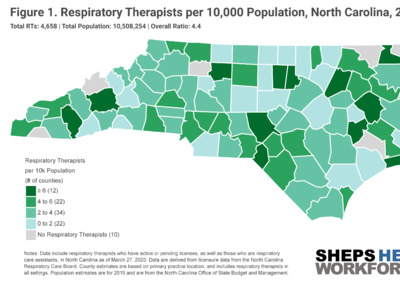
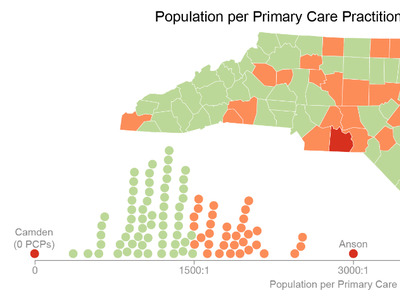
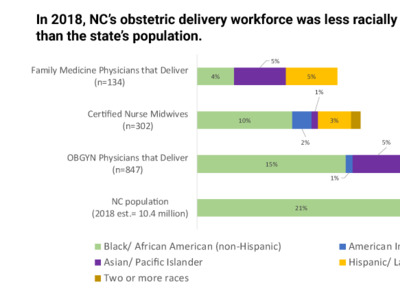
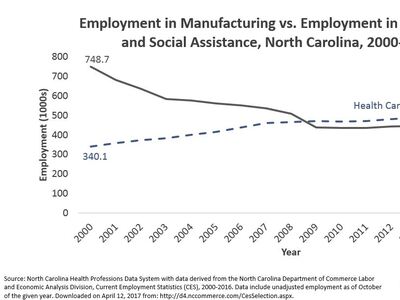
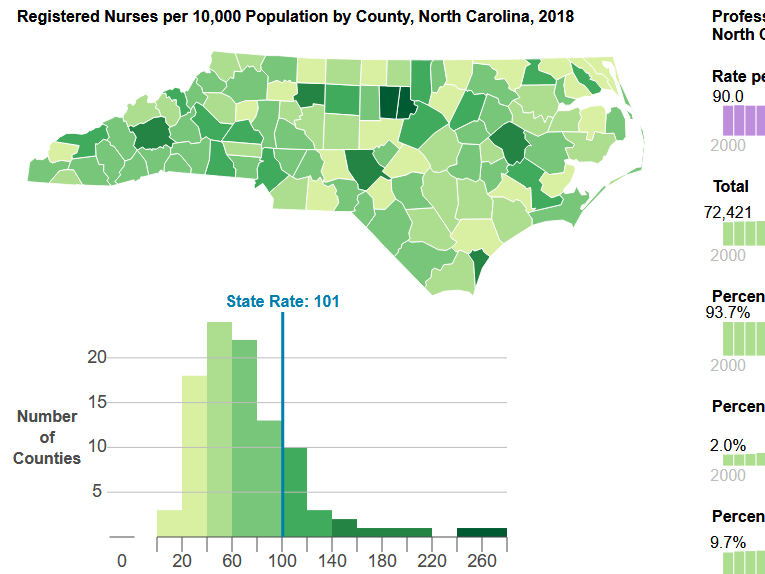
As North Carolina prepares for possible future waves of COVID-19 cases requiring hospitalization, @WorkforceNC is committed to providing data on the availability of critically needed health professionals, such as critical care nurses, respiratory therapists, infectious disease specialists and primary care access. Health systems in North Carolina are acting quickly to boost the numbers of health care professionals, ICU beds, and equipment. This blog post represents the best available data as of May 21st, 2020.
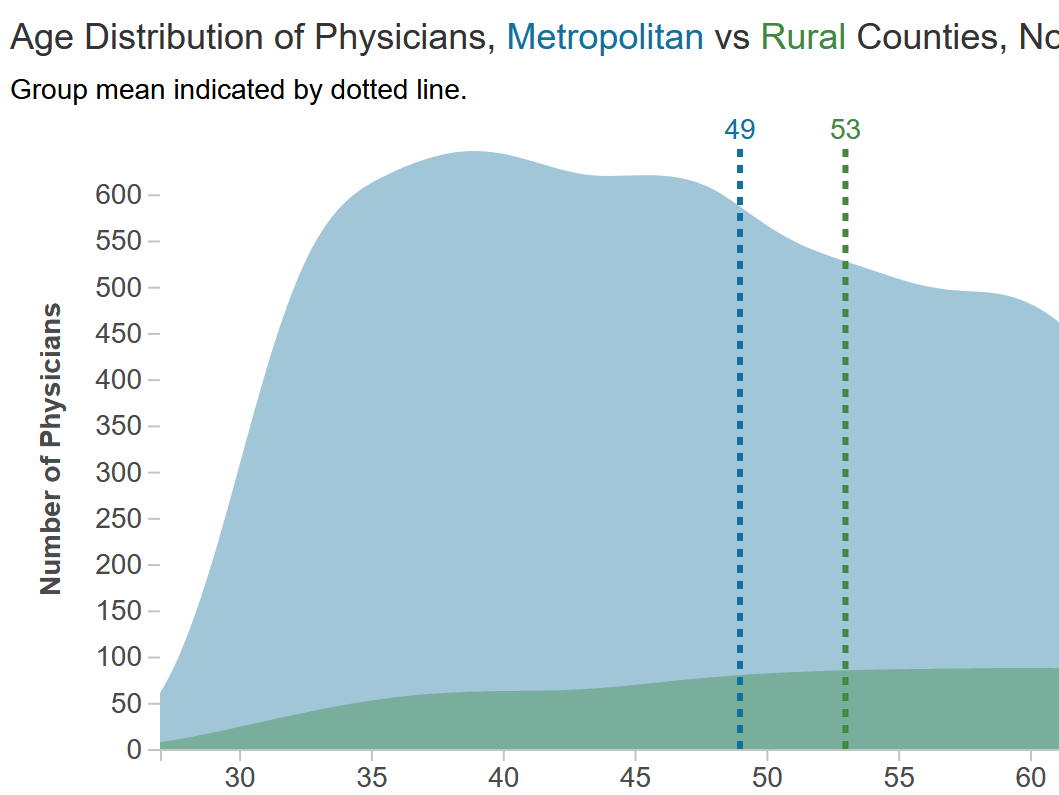
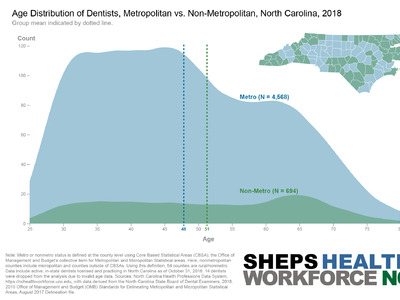
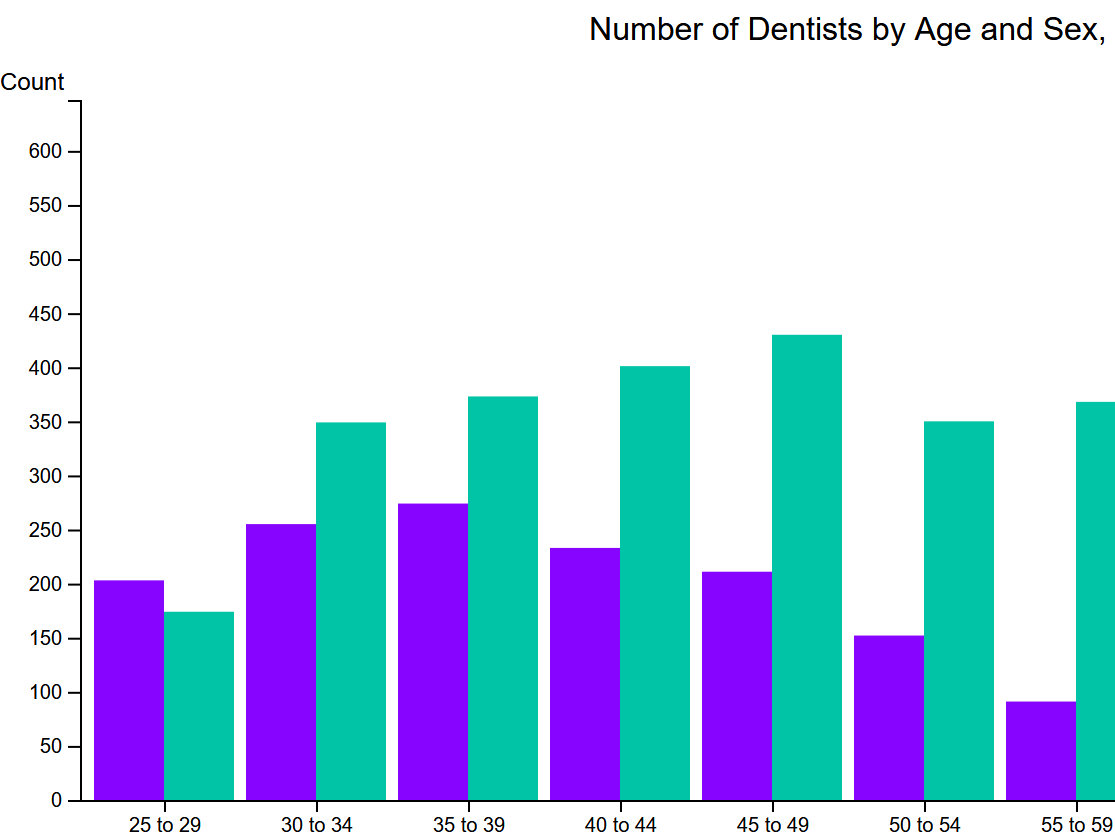
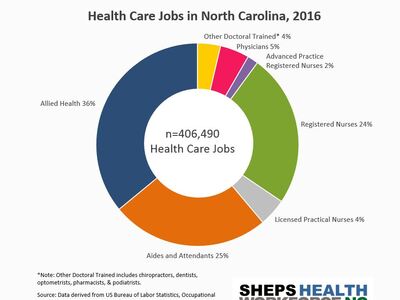
While North Carolina’s early social distancing and stay-in-place measures have flattened the curve, much about COVID-19 epidemiology is unknown. Subsequent outbreaks of COVID-19 still have the potential to strain the health care system’s critical care and emergency medicine capacity, particularly in rural areas. Critical care physicians, or intensivists, are board-certified physicians who care for complex and critically ill patients in the ICU, often coordinating a team of nurses, physical therapists, respiratory therapists, and pharmacists. An intensivist completes a residency in pulmonary medicine (most common), pediatrics, or surgery, followed by a fellowship in critical care medicine. They manage ventilator use, invasive monitoring techniques, resuscitation, life support and end-of-life care.
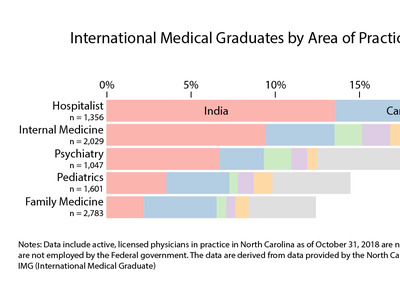
Even before the pressures of a pandemic, studies reported a shortage of critical care physicians. COVID-19 has the potential to significantly increase the demand on ICUs and the physicians who staff them. COVID-19 patients have an average length of stay of 8-12 days in the hospital, longer than the average stay of 5 days. With a properly staffed team of NPs, PAs, CNs and CRNAs, an intensivist can generally manage 6 patients each—in a surge, this ratio can flex to 1:8. The Society of Critical Care Medicine (SCCM) has recommended hospitals adopt a tiered staffing model in which one experienced critical care physician supervises four ICU teams, better utilizing providers with less ICU training. In hospitals with an “open unit,” hospitalists often already help cover ICU and step-down patients. Similarly, family medicine and internal medicine doctors, especially those who were recently residents, can flex up to do hospitalist work. Individual hospitals and health care systems should plan for increased resource use given their unique staffing configuration.
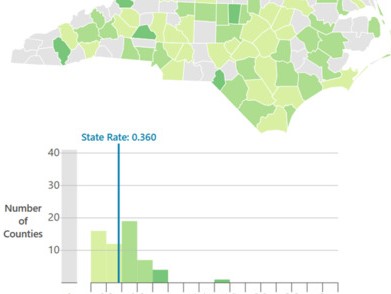
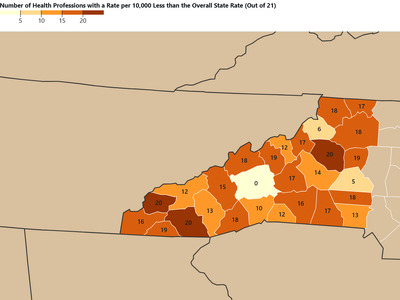
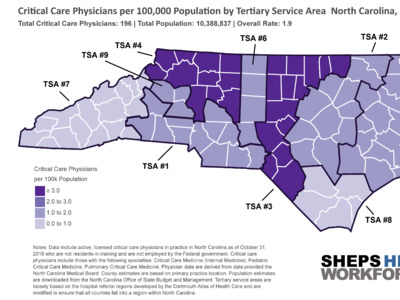
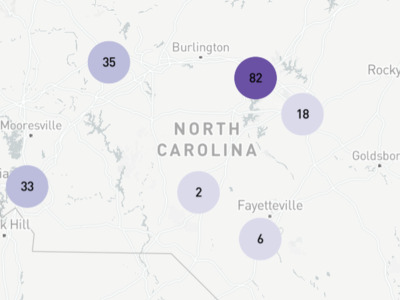
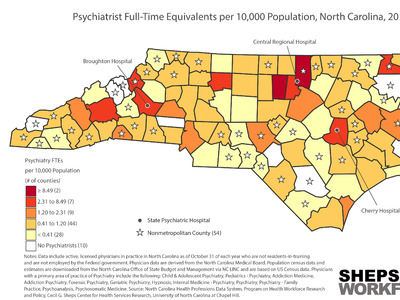
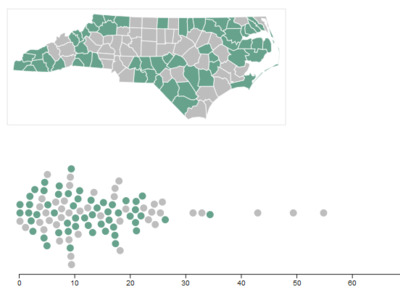
The map below shows the supply of critical care medicine physicians relative to population by Tertiary Service Areas (TSAs). TSAs are groups of counties that reflect where patients might be sent for specialty care.[1] TSA #3, which contains the cities of Chapel Hill and Durham, had the highest proportion of critical care physicians, at 3.9 per 100K population. TSA #4, which contains the city of Winston-Salem, also had a higher ratio, at 3.2 per 100K population. TSA #7, which contains the city of Ashville, had the lowest ratio, at .9 per 100K population.
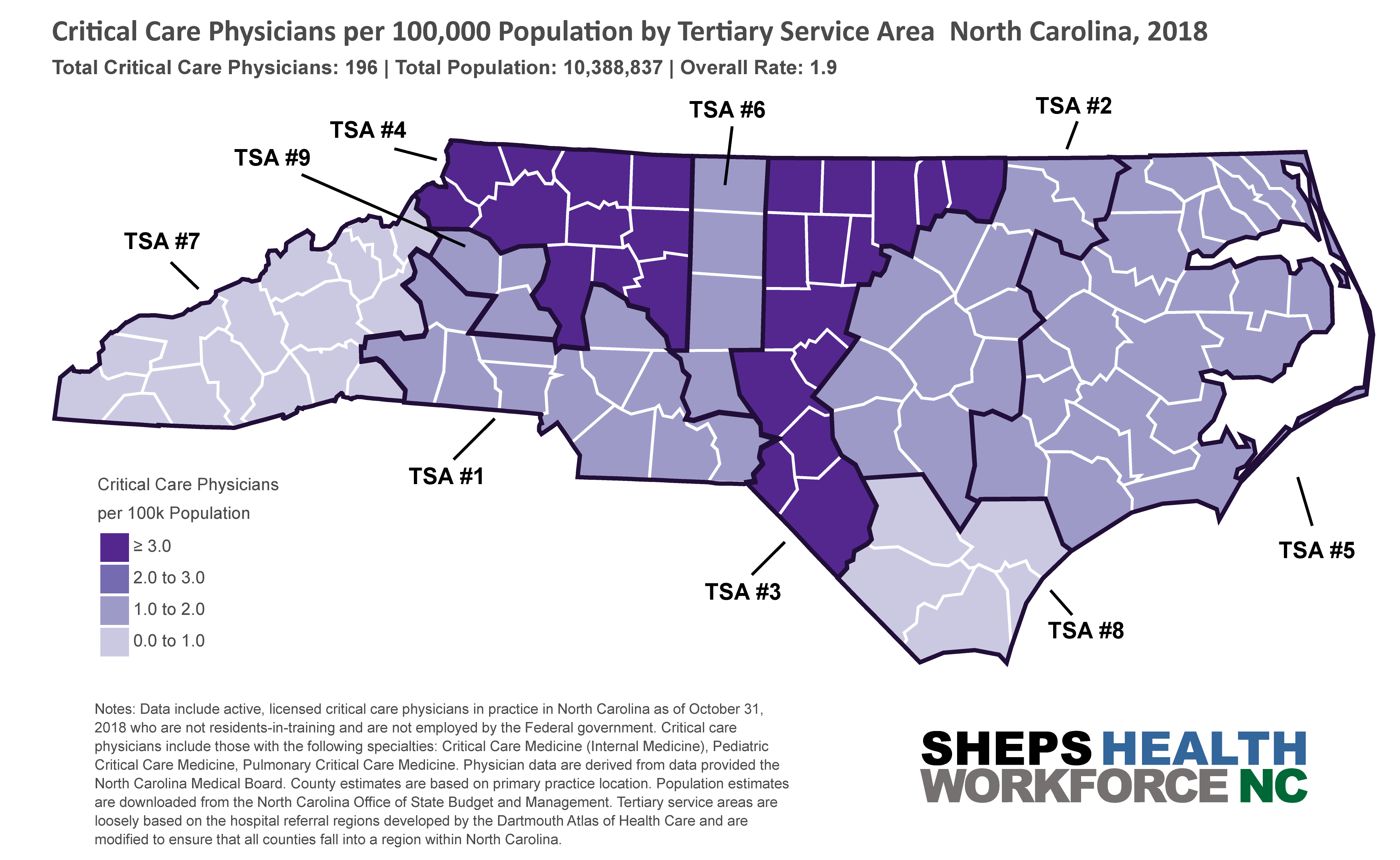
In a national model from late March, Array Advisor estimated that by the time of peak resource use—mid-April according to IHME model— NC would have a shortage of 329 critical care physicians, the fifth worst shortage in the nation. However, according to a recent policy brief from a group modeling COVID-19 impact in the state, NC’s early and aggressive precautions paid off, paving the way for a gradual reopening. This optimistic outlook is still contingent on continued containment strategies such as testing, contract tracing, social distancing measures and limiting gathering size.
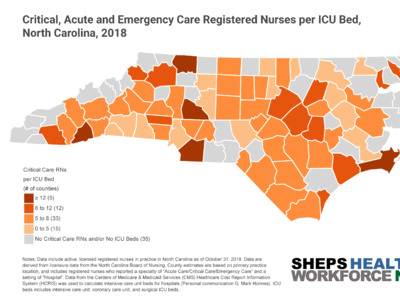
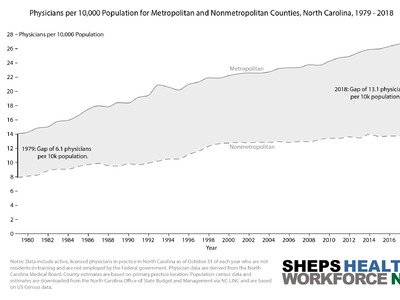
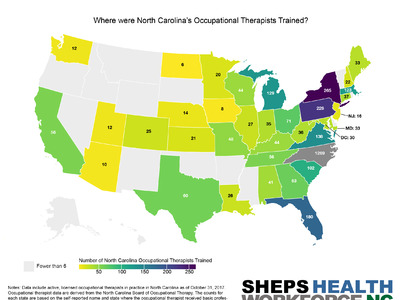
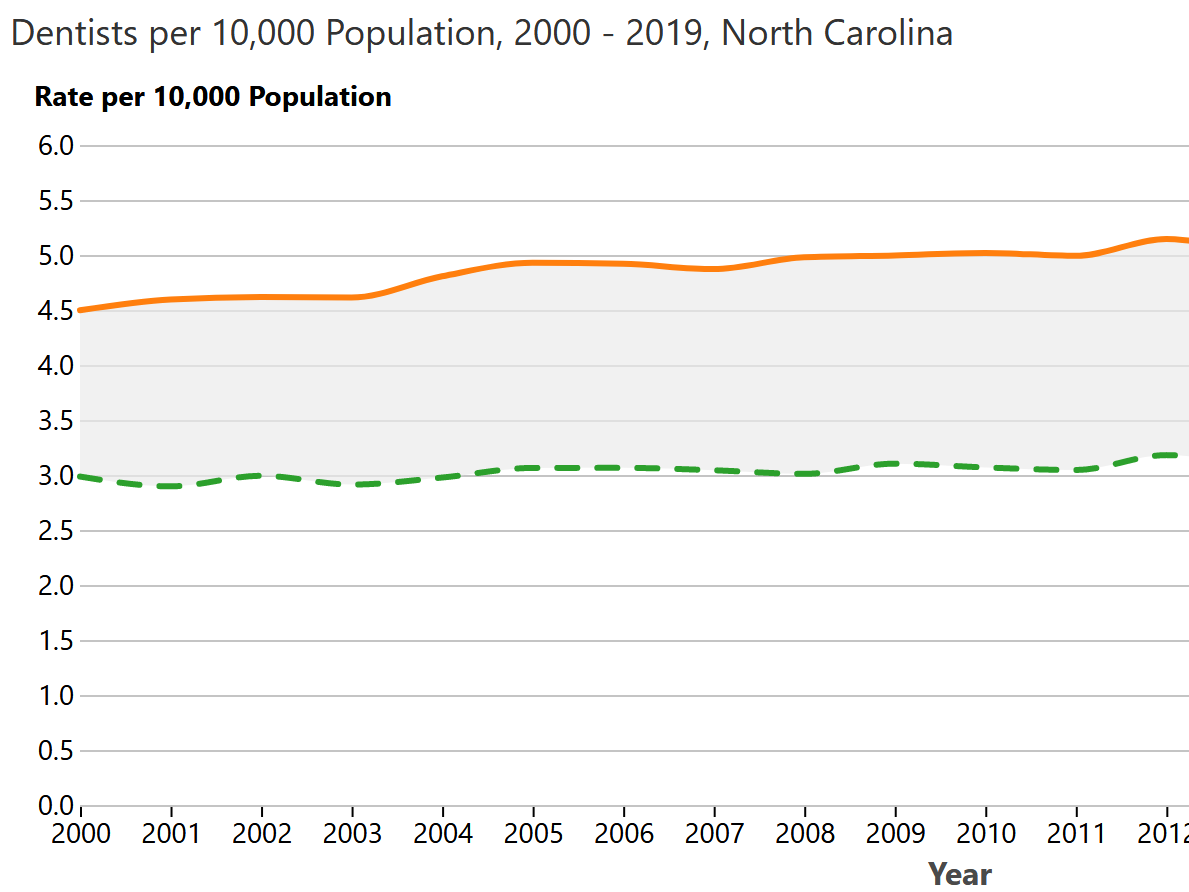
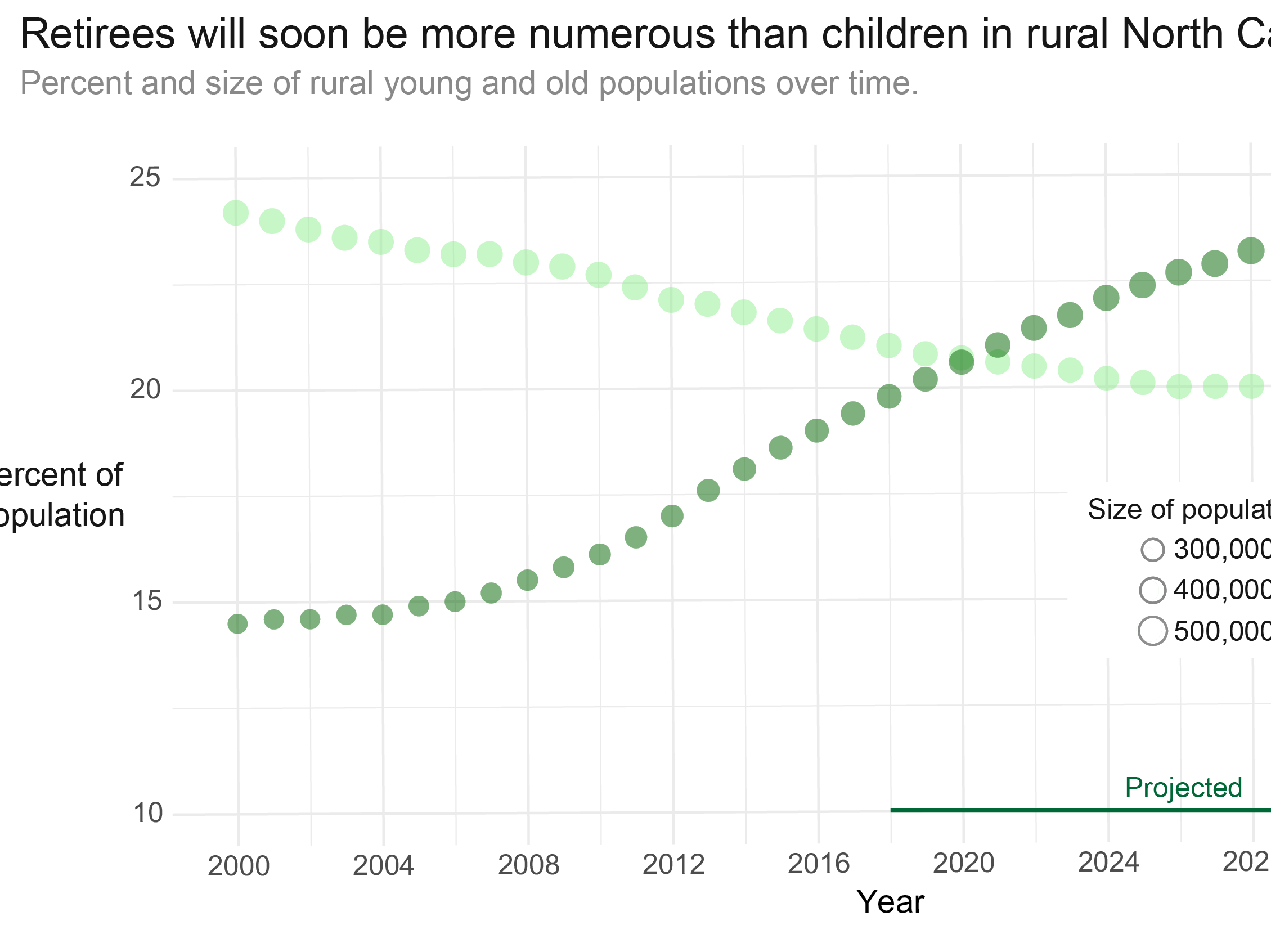
Coronavirus cases were initially concentrated in metropolitan centers but have rapidly spread across 99 out of 100 counties in the state. NC’s Department of Health and Human Services has put out a call for nurses, clinicians, and other types of health care workers to bolster the health care workforce. The state seeks to surge capacity of the health workforce in addition to ICU beds. In March, a policy brief suggested that rural hospitals have lower occupancy rates compared to urban areas, and may be able to absorb more ICU patients in a surge. However, more recent data indicate that as of May 15th COVID-19 cases per capita are now higher in rural areas in NC than in urban areas.
[1] North Carolina’s Tertiary Service Areas (TSAs) are county-based versions of Hospital Referral Regions developed at the Dartmouth Atlas Project. Hospital referral regions (HRRs) boundaries are variable geographic units - TSAs aggregate this to the county level to create county blocks of referral areas. More information on the Dartmouth Atlas Project and HRRs can be found here.