North Carolina’s Supply of Critical Care Nurses are Crucial to the State’s COVID-19 Response
By Erin Fraher, Allie Tran, Julie Spero, Heather Wilson
Apr 1, 2020
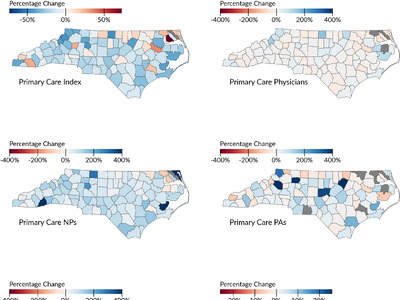
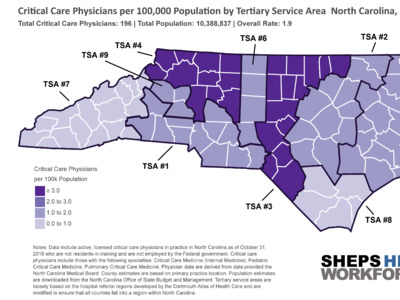
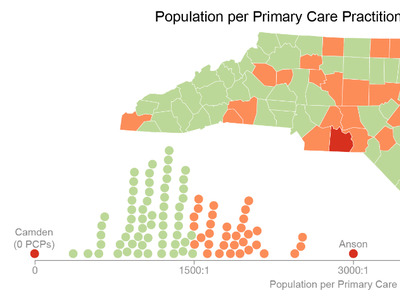
As North Carolina (NC) prepares for a rising number of COVID-19 cases, @WorkforceNC is committed to providing data on the availability of needed health professionals. Check out our blogs on infectious disease physicians and primary care access.
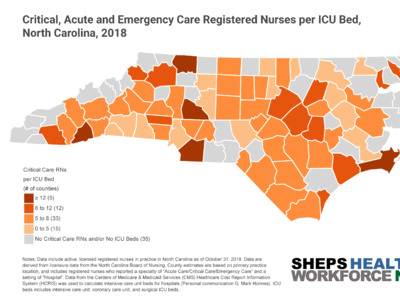
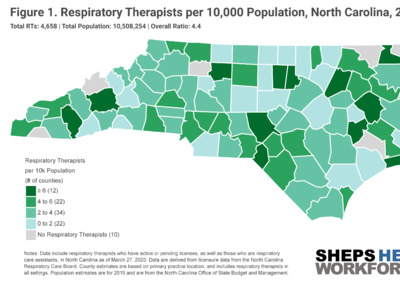
High numbers of COVID-19 patients will strain the health care system’s critical care and emergency medicine capacity, sharply increasing demand for hospital Intensive Care Units (ICU) beds and staff. Along with ICU beds, ventilators and personal protective equipment (PPE), NC needs the nursing workforce to care for the high influx of critically ill patients. Critical care nurses closely monitor and evaluate patients, manage advanced technologies, administer treatments, assist in procedures, and collaborate with respiratory therapists and physicians to coordinate advanced care for patients with respiratory failure and other life-threatening conditions.
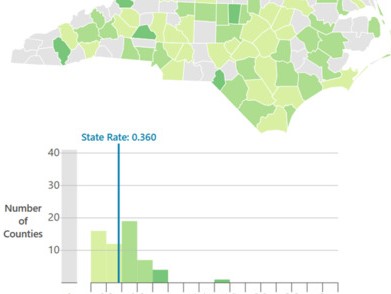
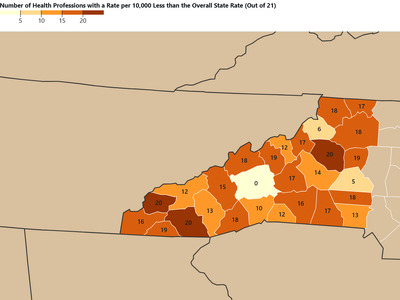
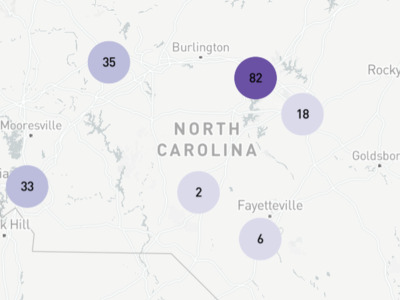
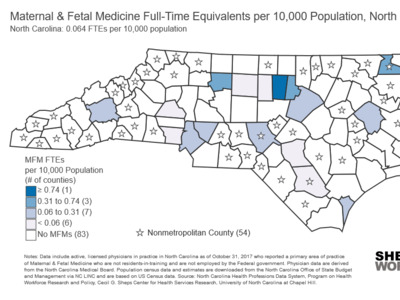
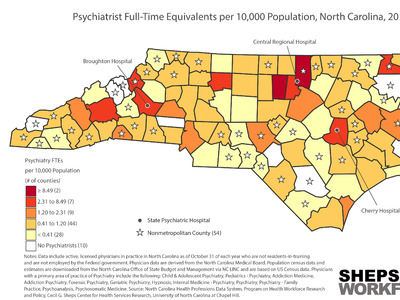
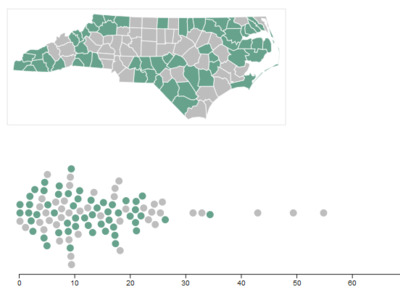
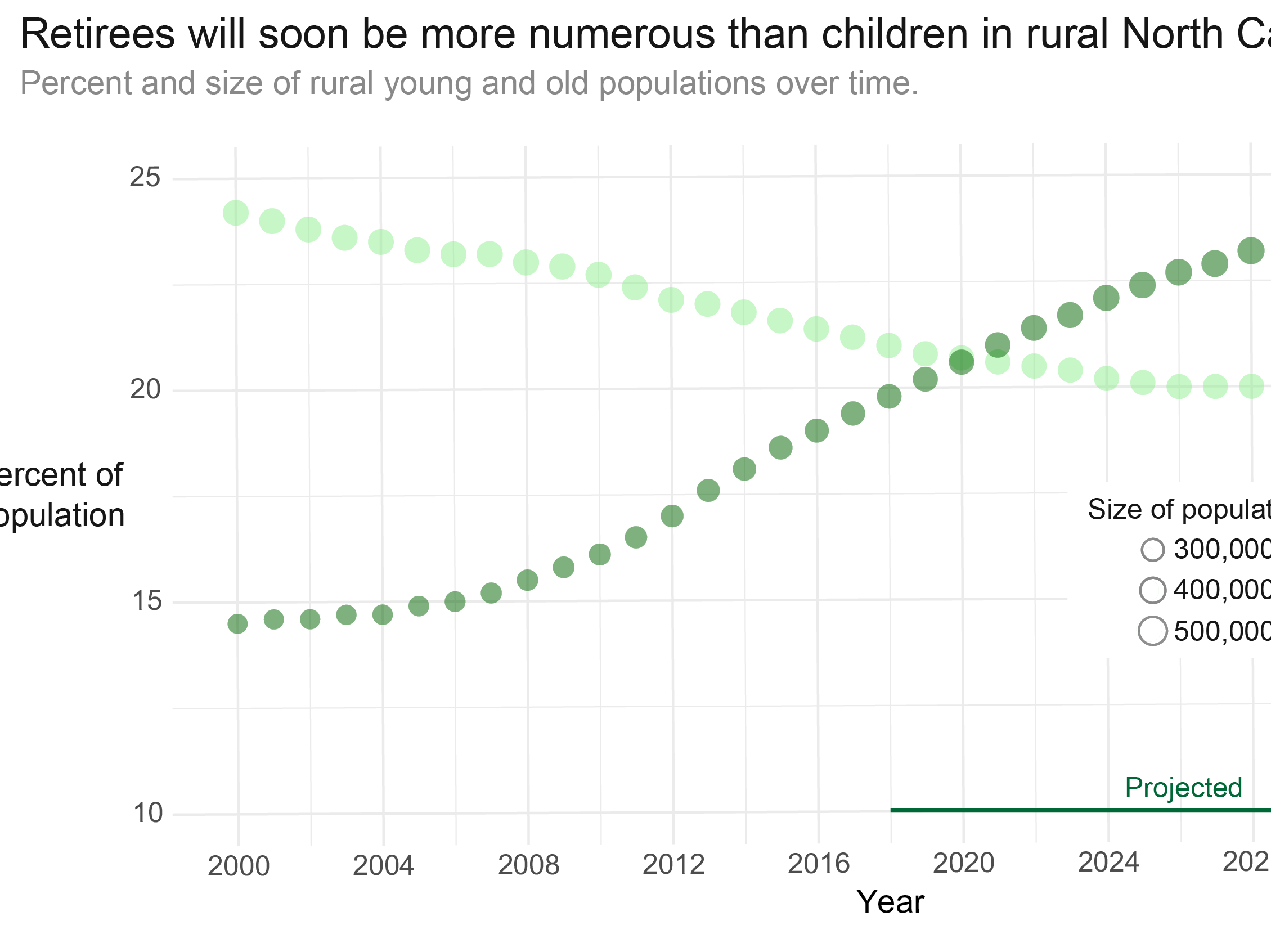
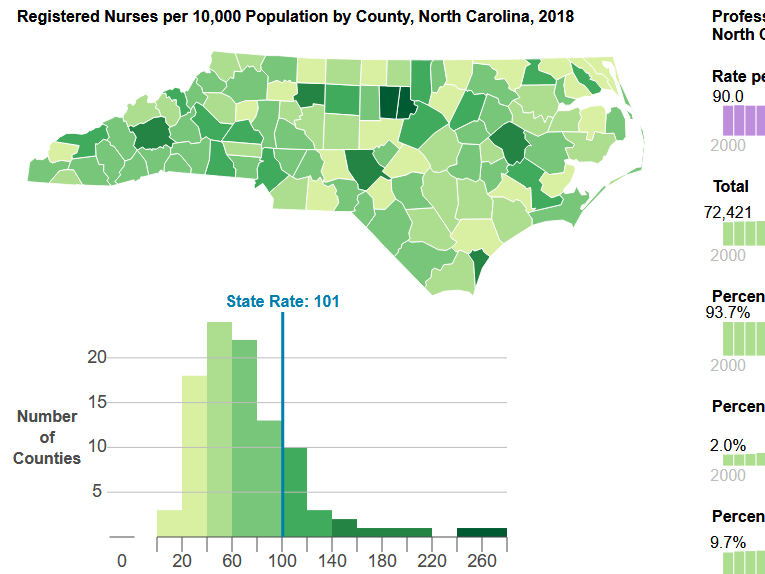
ICUs are typically staffed with one nurse for every one or two patients—in a surge situation, this ratio can increase to 1:3. Surge staffing and the shortage of trained ICU nurses could pose significant challenges for the state, especially if outbreaks occur in counties with fewer critical care nurses. NC’s critical, acute and emergency care workforce is densely clustered in counties with academic health centers such as Orange, Durham, Buncombe, and New Hanover. Some rural counties—such as Swain and Mitchell—also have a higher density of critical care nurses, despite not having an ICU. Critical care nurses in these areas likely work in step-down, post-operative, progressive care and telemetry, air/ground transport and rapid response teams, and could also support surge staffing to meet the needs of critically ill COVID-19 patients.
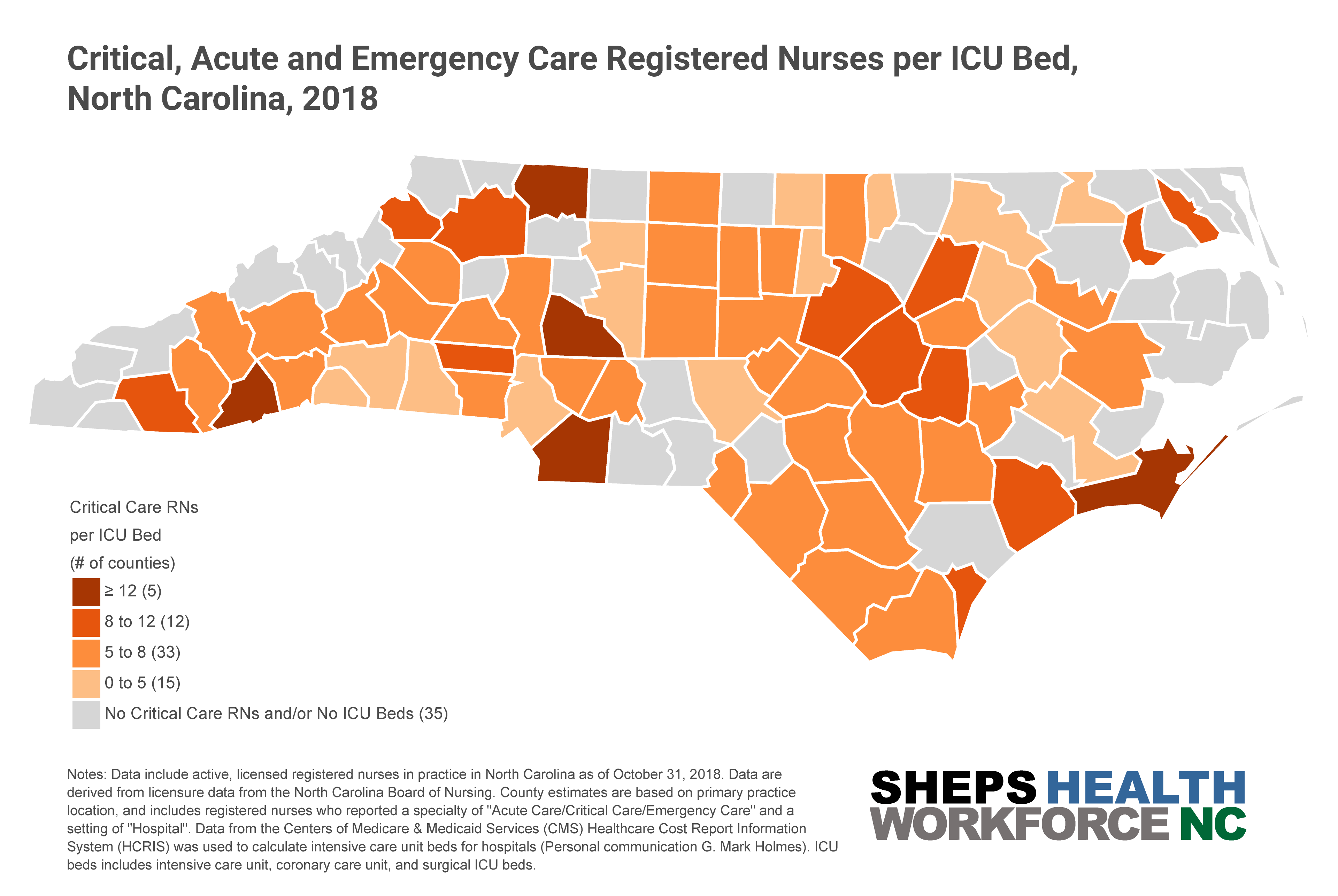
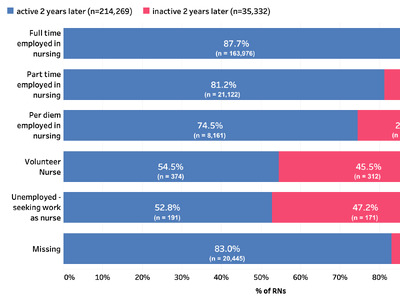
To increase the existing workforce and support the anticipated surge of critically ill COVID-19 patients, places in NC with few ICU nurses may need to incentivize RNs to relocate to these areas or cross-train existing staff, such as emergency and acute care RNS, peri-operative RNs (e.g., PACU and OR RNs), nurse anesthetists, and acute care nurse practitioners, to care for ICU-level patients. The Society of Critical Care Medicine (SCCM), American Association of Critical Care Nurses (AACN) and North Carolina Area Health Education Center (NCAHEC) provide several resources to support cross training non-ICU clinicians to care for patients with COVID-19. These online trainings, geared for those without formal ICU knowledge, focus on assessment and management of patients with respiratory failure, ventilator settings/protocols, and infection control strategies.
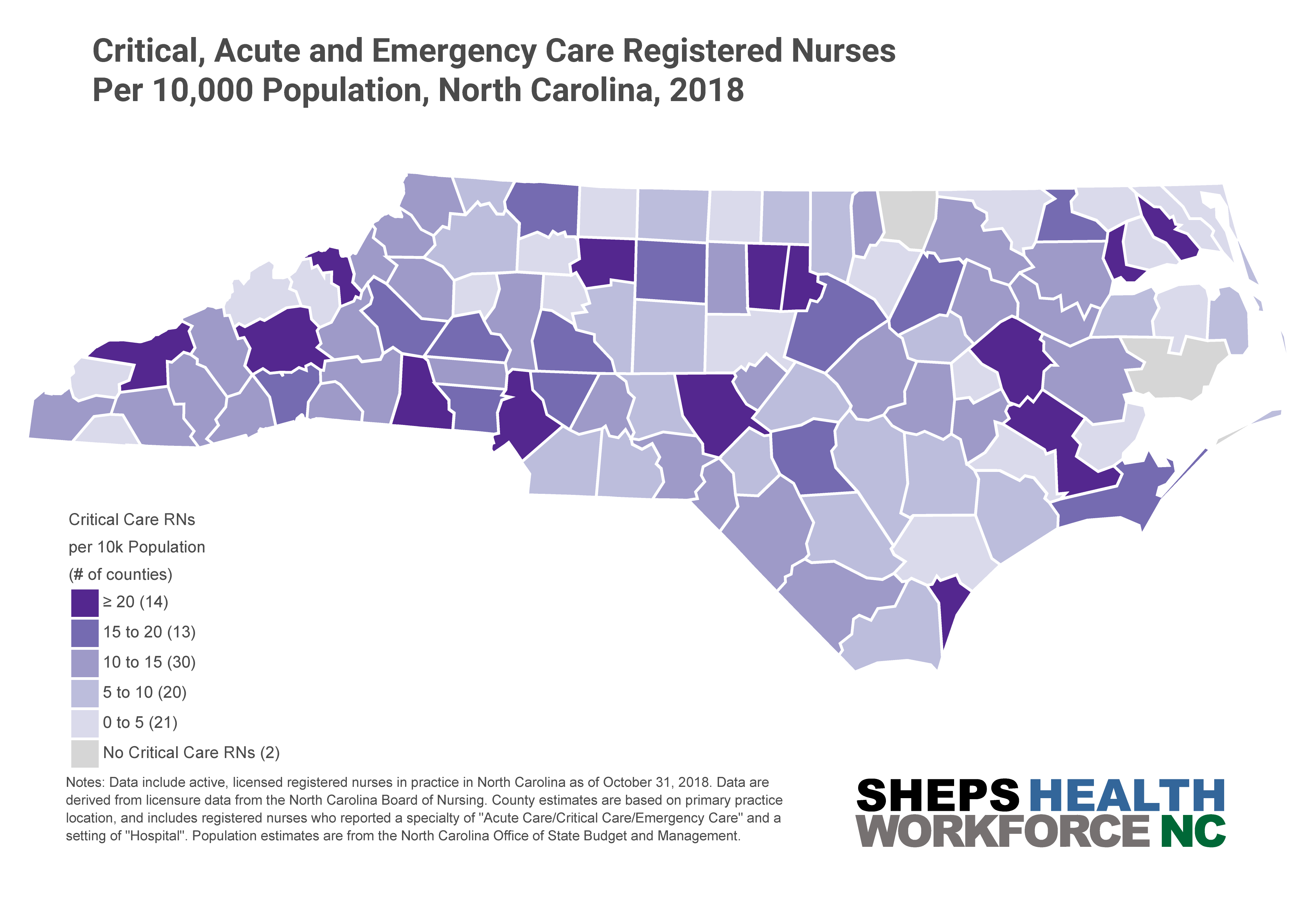
Coronavirus cases were initially concentrated in metropolitan centers but have rapidly spread across many counties in the state. NC’s Department of Health and Human Services has put out a call for nurses, clinicians, and other types of health care workers to bolster the healthcare workforce. The state seeks to surge capacity of the health workforce in addition to ICU beds. A recent policy brief suggested that rural hospitals have lower occupancy rates compared to urban areas, and may be able to absorb more ICU patients in a surge.