North Carolina’s Respiratory Therapist Workforce: Availability to treat COVID-19
By Erin Fraher, Evan Galloway, Julie Spero, Heather Wilson
Mar 25, 2020
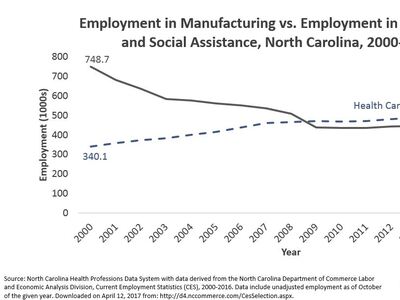
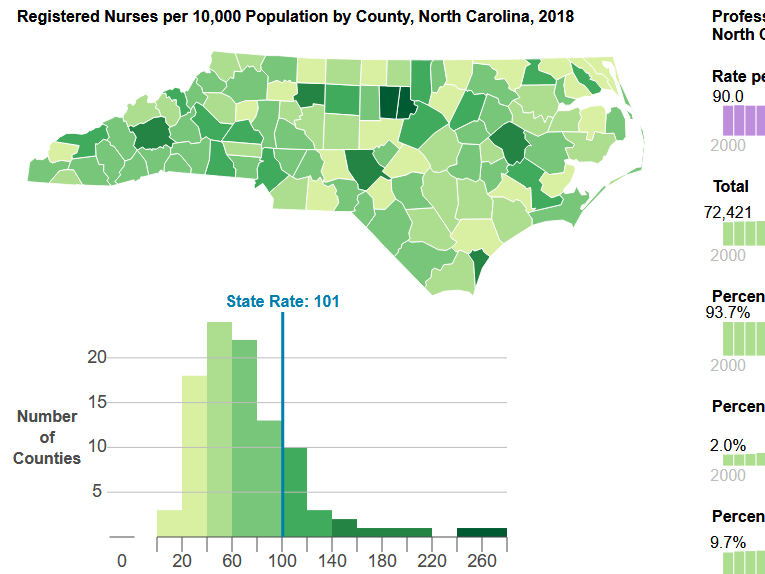
As North Carolina prepares for a rising number of COVID-19 cases requiring hospitalization, @WorkforceNC is committed to providing data on the availability of critically needed health professionals, such as critical care nurses and infectious disease specialists. Health systems in North Carolina are acting quickly to boost the numbers of health care professionals, ICU beds, and equipment. This blog post represents the best available data as of April 3rd, 2020.
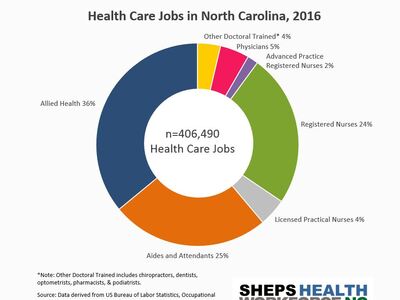
NPR recently reported that 2% of those who contract the coronavirus develop respiratory issues that require a ventilator. In addition to concerns about a shortage of ventilators, North Carolina needs the skilled medical workforce required to staff ventilators. Respiratory therapists (RTs) are associate-degree-educated health professionals who care for patients that have trouble breathing, including operating and managing ventilators. While many work in hospital intensive care units (ICUs) about 15% of NC’s RTs work in other settings, like home health and nursing homes.
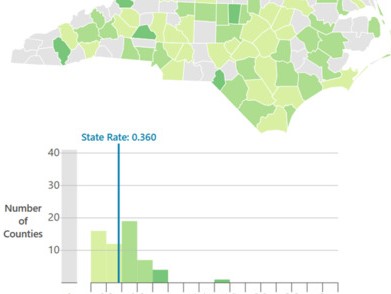
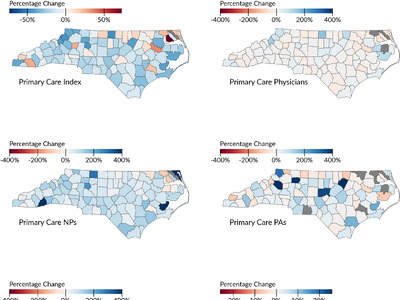
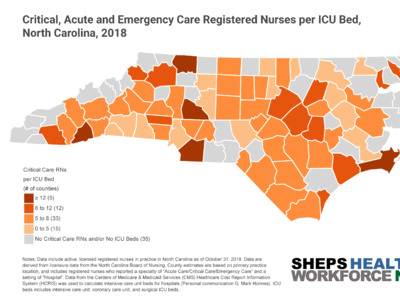
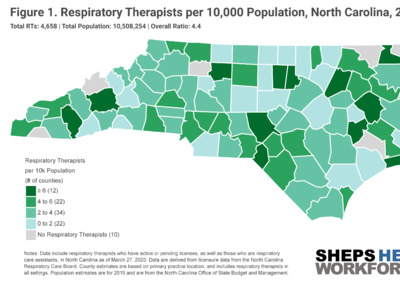
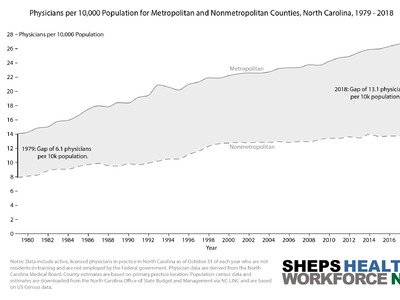
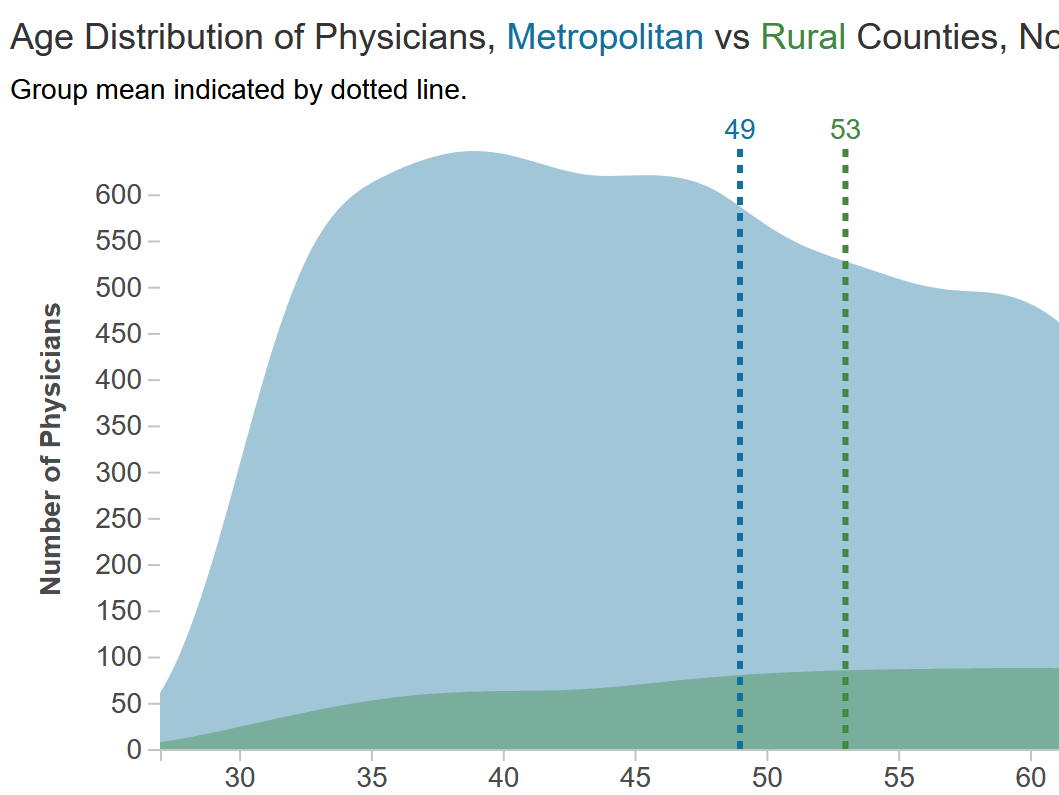
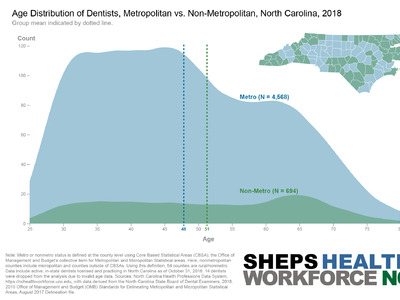
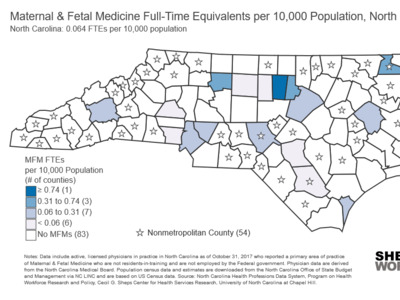
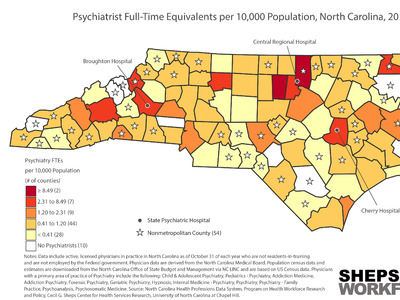
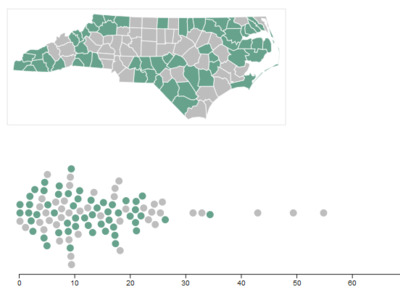
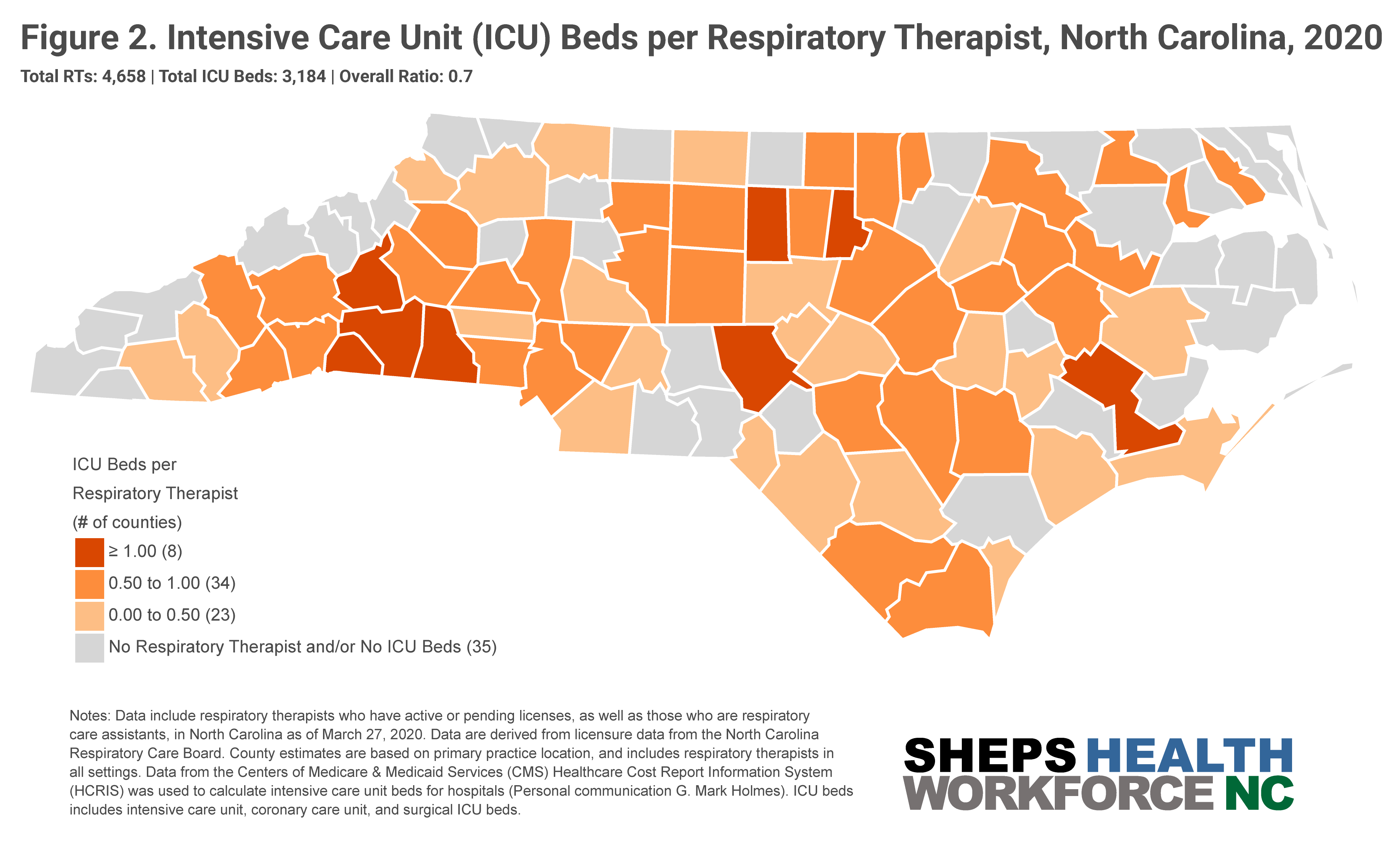
Experiences in Italy, China and the current outbreaks in Washington, California and New York have demonstrated that COVID-19’s impacts will likely be concentrated geographically. This makes it critical to understand how the state’s supply of RTs and ICU beds varies by county. Figure 1 shows the RT workforce is concentrated in metropolitan areas with large academic health centers.
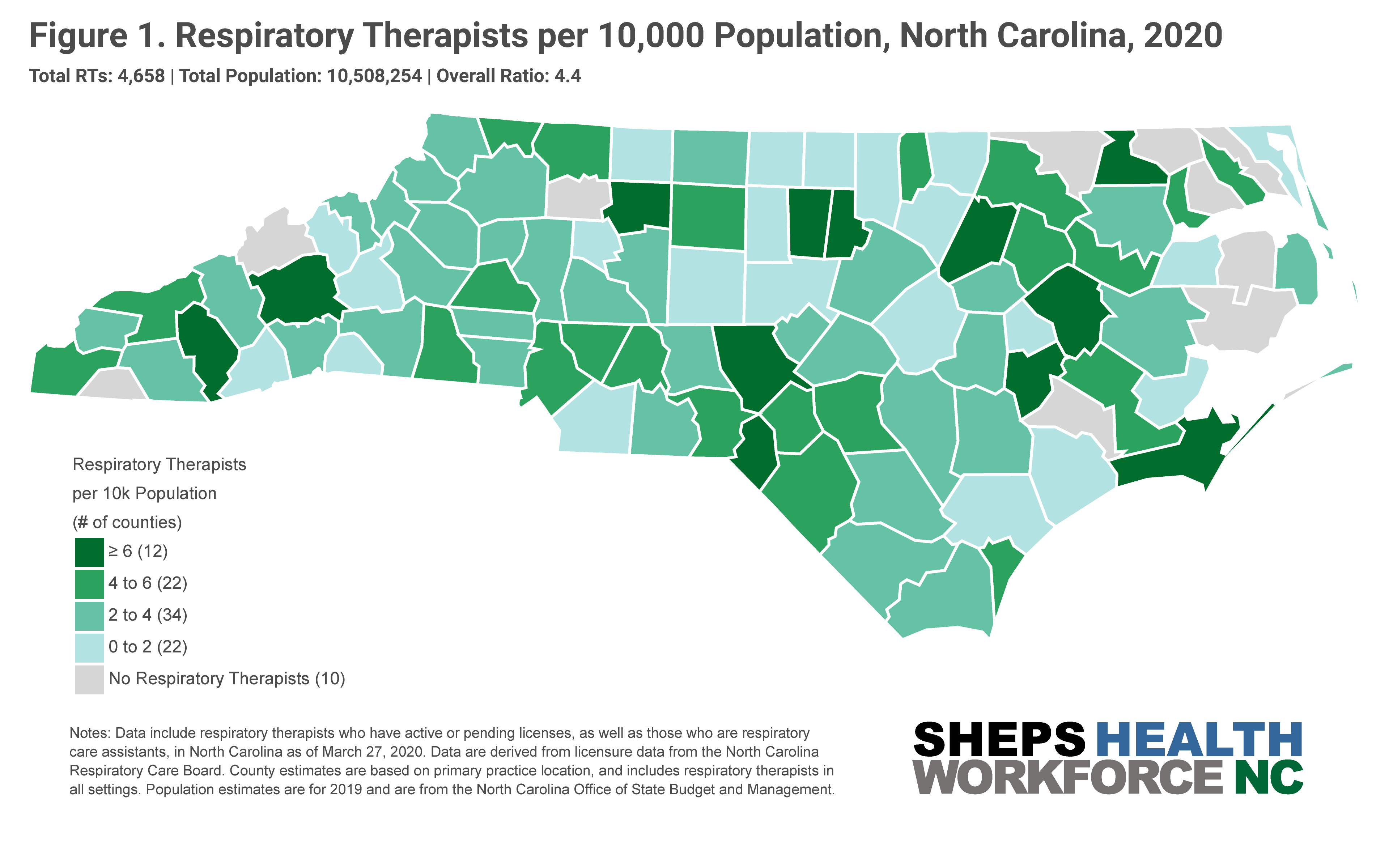
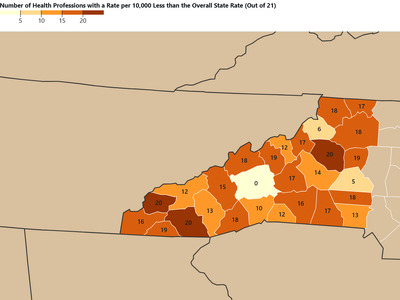
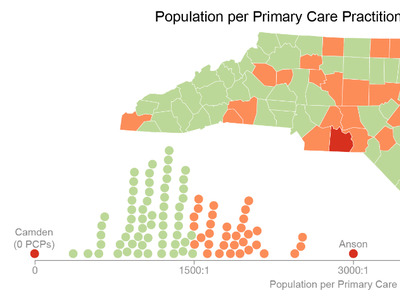
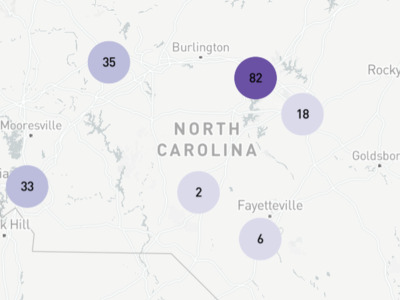
35 counties in NC have no ICU beds and/or no RTs (Figure 2). Eight counties have an ICU bed to RT ratio of greater than one, meaning these counties have more ICU beds then RTs —Alamance, Durham, Craven, Moore, Cleveland, Rutherford, Polk, and McDowell. The number of ventilators an RT can safely manage at one time depends on patient acuity. Data suggest that for patients with highly acute illness, the safe ratio is one RT to four ventilators, and with less acute patient illness the ratio may increase up to one RT per nine ventilators.
NC’s Respiratory Care Board (NCRCB) has acted swiftly to surge the state’s potential workforce. The Board has waived continuing professional development (CPD) and late fees, postponed background checks, allowed RTs whose licenses have expired within the last 3 years to renew their license without paperwork, and allowed RTs between 3 and 5 years out of practice to renew by a signed application. Over the past few weeks, the board has also brought 90 2nd-year Respiratory Care Assistants (RCAs) into practice, and is processing out-of-state reciprocity licenses in 48-hours.
The Board recently received 70 responses to a survey they fielded asking about RT capacity in the state, representing licensed hospitals, home care, nursing homes and long-term care facilities in NC. 70% of respondents reported that they were either “very worried” or “extremely worried” about the impact of coronavirus on staff. Survey responders indicated a need for 765 additional respiratory therapists. The actual number of RTs needed in the state is likely higher since 40% of licensed hospitals did not respond to the survey.
North Carolina’s workforce that is immediately available to practice is comprised of 4,658 RTs with active licenses. Roughly 500 RTs have an active license but are currently unemployed and another 50 are retired. These licensees could quickly join the state’s workforce; but even when combined with the 90 new Respiratory Care Assistants, they won’t be able to meet the projected demand of 765 additional RTs. A separate pool of 527 RTs with licenses that expired fewer than 3 years ago could rejoin NC’s workforce with ease given current board actions, but it is unclear how many will do so.
As demand surges, the state will likely continue to add ICU beds to meet that demand. Policy makers may need to consider ways to encourage RTs to relocate to needed locations. Respiratory therapists can also provide some services in a telehealth setting, such as diagnostic evaluation, sleep testing, disease prevention and rehabilitation. Hospitals and health systems should make plans now about how they could utilize other trained staff like Certified Registered Nurses Anesthetists and critical care RNs to help support ventilator patients.
ProPublica recently reported hospitals using ventilators to support more than one patient. The American Association for Respiratory Care (AARC)—in conjunction with a number of other leading critical care organizations—has counseled against sharing ventilators, as it cannot be done safely with current equipment, and in the case of COVID-19 patients specifically, “could lead to poor outcomes and high mortality rates for all patients.”