Retention of Registered Nurses: A Brief Report on Interventions to Increase Retention in the Nursing Workforce
By Catherine Moore, Brooke Lombardi, Erin P. Fraher
Sep 17, 2025
Introduction
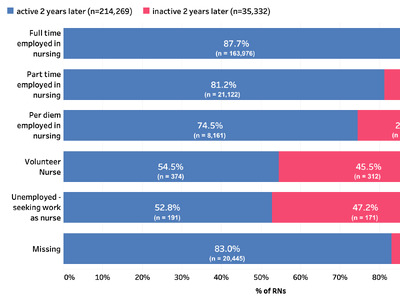
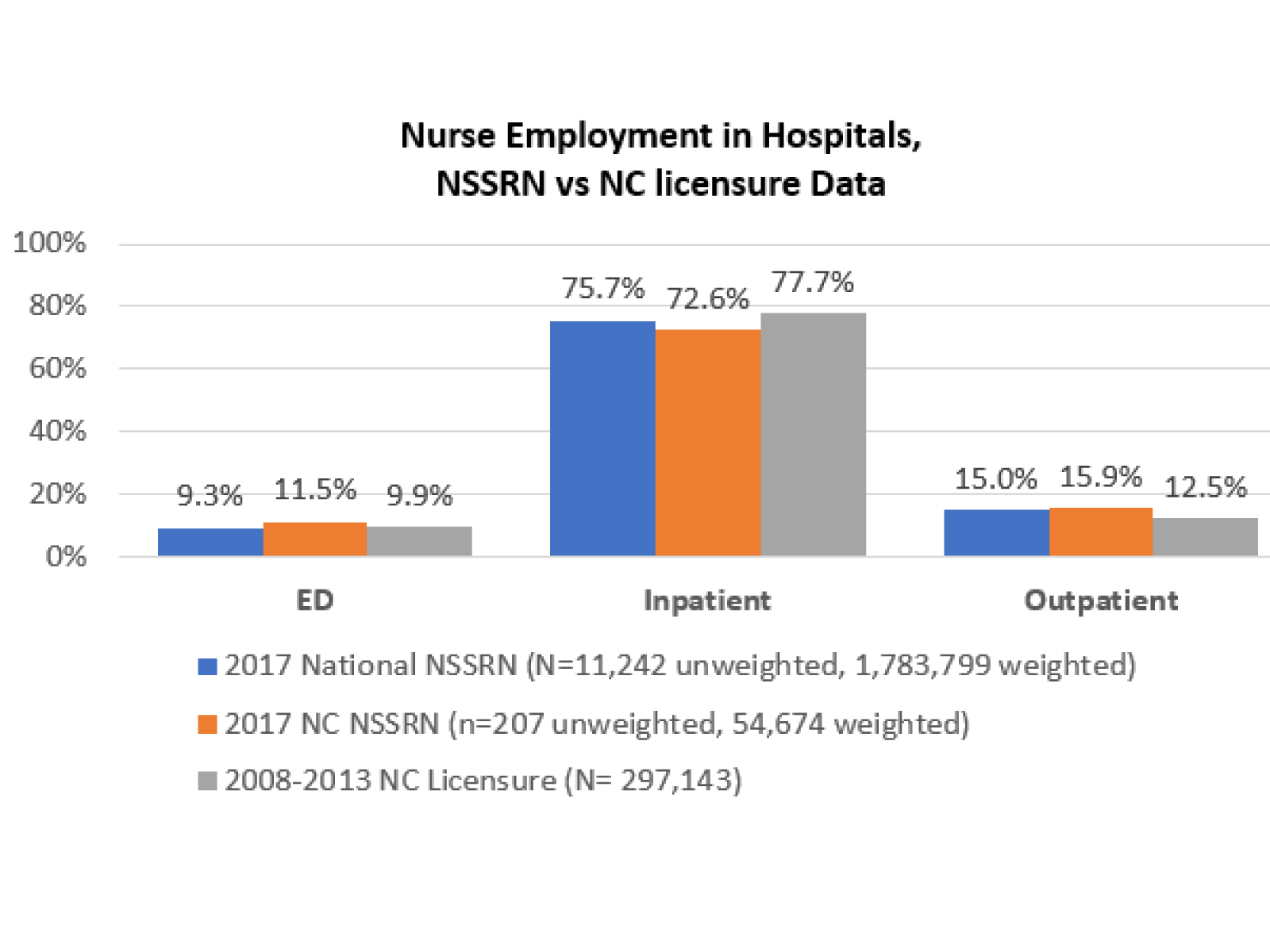
North Carolina (NC) is projected to face a shortage of almost 12,500 registered nurses (RNs) by 2033.1 A 2023 survey of more than 1,000 NC health care facilities and 80 education programs conducted by the NC Health Talent Alliance found that 1 in 6 RN positions in the state were unfilled.2 Nationwide, RN staffing intensity (the ratio of RNs to other nursing personnel) in hospitals has decreased since 2021, consistent with findings from Auerbach et al. (2024) which suggest that although overall nurse supply in the United States is increasing, most of the growth is taking place outside of hospitals.3
A recent report by NSI Nursing Solutions (2025) estimated a cost of $61,110 for turnover of one bedside nurse and a three-month timeframe to recruit an experienced RN.4 However, research by Jones (2008) estimated an even higher cost of nurse turnover, ranging from $82,000 to $88,000 depending on RN experience.5 Although estimates of the cost of nurse turnover vary depending on the methodology used, nurse turnover is costly and hiring a new RN is time consuming.6 Factors associated with nurse turnover include burnout, insufficient staffing, inadequate compensation and benefits, lack of professional development opportunities, issues with workplace culture and management, safety concerns, and health/mental health related concerns.7,8 In NC, a recent analysis examining exits from the NC RN workforce found that the percent of nurses who left the workforce increased from 13.9% in 2019 to 15.1% in 2023.9 Given the cost associated with nurse turnover, this increase in exits from the NC RN workforce requires attention.10
International calls have been made to prioritize programs and strategies to recruit and retain nurses in the workforce.11,12,13 Within NC, the 2024 NC Institute of Medicine (NCIOM) nursing workforce report14 outlined several strategies to sustain and retain nurses in the NC workforce, including strategies that can be implemented within nursing units and more broadly at the organizational level:
- identifying opportunities for nurses to participate in educational advancement, leadership, mentoring, and preceptorship
- decreasing the experience of high workload and documentation burden for nurses
- strengthening nurse transition to practice efforts and early career development across all care delivery settings
- protecting nurses from violence in the workplace
- increasing awareness and support for the mental health of nurses
- creating robust systems that involve nurses as leaders in decision making This brief summarizes the results of a review of systematic reviews focused on nursing retention interventions that have been quantitatively evaluated. In this brief, we summarize findings from the literature on retention interventions and discuss their implications for NC RN workforce partners such as employers, policy makers, NC AHEC, and the NC Center on the Workforce for Health, who have an interest in promoting methods to retain the NC nursing workforce.
Methods
This review focused on systematic reviews and meta-analyses in English published after 2020 that quantitatively measured nursing turnover, intention to stay or leave, and retention. The research team, which included a health sciences librarian, conducted literature searches in CINAHL Plus with Full Text (EBSCOhost), Cochrane Database of Systematic Reviews, PubMed, and Scopus (Elsevier) using multiple relevant subject headings (e.g., “healthcare worker retention” or “turnover”) and key words (e.g., “retention,” and “interventions,” AND “nurse”). The original searches yielded 1,453 articles which were reviewed by the research team. First, two researchers independently screened the titles and abstracts for inclusion and exclusion criteria. Studies were included if: 1) the study subjects included nurses; 2) the intervention’s purpose focused on nurse retention; 3) the study’s context was within healthcare; 4) and the outcomes included a quantitative measurement of retention. Exclusion criteria applied included: 1) systematic reviews that included qualitative-only research; 2) scoping reviews; 3) studies on students 4) studies on graduate nurses (not yet licensed); 5) studies on nursing faculty; 6) studies on advanced practice registered nurses; 7) and studies on more than one healthcare clinician. Next, the same researchers independently screened 17 full-text references for inclusion and resolved any discrepancies through discussion. The final sample included six systematic reviews published between 2020 and 2024. The research team extracted data from each review including author(s) name, year of publication, review objective, setting type, level of intervention (unit-level or organizational-level), number of quantitative studies that measured retention, measure(s) of retention, and findings.
Findings
The final sample of six reviews9,15,16,17,18,19,20 represent 67 studies that measured nurse turnover, intention to stay or leave, and retention. While all reviews included studies of nurse outcomes in hospitals, only one review (Mohamed & Al-Hmaimat, 2024) included a study of retention in long term care settings.21 Retention was not consistently measured or reported across studies in the reviews. Measures of retention included turnover intention, intention to leave, and intention to stay using a variety of validated and researcher-created survey tools (Table 1).
Table 1. Systematic Review Characteristics
| Author(s) | Published year | Number of Quantitative Studies | Review objective | Nursing setting type | Intervention | Level of Intervention | Tools for measuring workforce outcomes | Workforce outcomes |
|---|---|---|---|---|---|---|---|---|
| Aparício & Nicholson15 | 2020 | 2 | To determine if there is evidence to support preceptorship and clinical supervision programs in retaining nurses, and particularly newly qualified nurses (NQNs), in clinical practice. | Hospital-based settings | Clinical supervision program; Preceptorship program | Organizational | Validated 26-item Manchester Clinical Supervision Scale (MCSS) and Site coordinators tracked at one year after the hire date, each newly licensed RN was coded as retained, left voluntarily, or left involuntarily (injury or termination). | Intention to stay Retention rate |
| Conroy et al.16 | 2023 | 12 | To synthesize the relationship between transformational leadership style and staff nurse retention in hospital settings. | Hospital-based settings | Transformational Leadership (TL) | Unit | McCain's Intent to Stay Scale (n=2), O'Driscoll and Beehr Scale (n=2), Intention to stay Scale (n=2), Affective Commitment Scale (n=1), Organizational Commitment Questionnaire (n=1), Anticipated Turnover Scale (ATS) (n=2), Turnover intention scale (n-1), Six-item turnover intention scale (n=1). | Intention to leave Turnover intention |
| Galanis et al.17 | 2024 | 8 | To synthesize and evaluate the association between organizational support and turnover intention in nurses. | Hospital-based settings | Organizational support | Unit | Turnover Intention Scale (n=33), Self-developed scales (n=5) | Turnover intention |
| Mohamed & Al-Hmaimat18 | 2024 | 5 | To determine the effect of successful completion of Nurse Residency Program on new nurses’ retention rates compared with new nurses who missed the Nurse Residency Program | Hospitals (4), long-term care facility (1) | Nurse residency program | Organizational | Not stated | Turnover rate Retention rate |
| Vázquez-Calatayud & Eseverri-Azcoiti19 | 2023 | 9 | To identify effective interventions that promote the retention of newly graduated registered nurses in the hospital setting and their components. | Hospitals | Combined [residency with one-to-one mentoring (n=4)], residency programs (n=3) and individualized mentoring (n=1), as well as diversified adaptive education [Instruction tailored to the skills, needs, and interests of NGRNs based on learning styles (n=1)]. | Organizational | Survey turnover intention (n=2) Intention to stay survey (n=1) |
Retention rate Turnover rate Intention to stay Turnover intention |
| Woodward & Willgerodt20 | 2022 | 31 | Examine current data on RN work outcomes for study quality, methods, and variables with specific attention to the inclusion of concepts related to equity and wellness. | Varied. Hospitals (10/34) or several hospitals within a region or system (9/34). Programs/hospitals across several states (6/34), secondary analysis of national dataset. | Nurse residency program (n=3), organizational support (n=2) | Organizational | Anticipated Turnover Scale (ATS) | Intent to leave Intent to stay Retention rate Turnover rate |
Nine themes emerged that focused on unit-level (implemented within the nursing unit) and organizational-level (implemented organization-wide) interventions to influence retention. Table 2 outlines the identified themes which were used to synthesize the findings. Unit-level interventions included transformational leadership (Conroy et al., 2023) and organizational support (rewards, favorable job conditions, assistance to perform tasks efficiently and manage stressful situations, support from the supervisor, meaningful recognition, shared decision making, and increased leadership involvement and support, and teamwork) (Galanis et al., 2024; Woodward & Willegerodt, 2022). Organizational-level interventions included preceptorship programs, clinical supervisor programs (Aparício & Nicholson, 2020), nurse residency programs (Mohamed & Al-Hmaimat, 2024; Vázquez-Calatayud & Eseverri-Azcoiti, 2023; Woodward & Willegerodt, 2022), adaptive education, individualized mentoring programs, combined residency and meeting points, best-fit orientation (Vázquez-Calatayud & Eseverri-Azcoiti, 2023), and organizational support (Magnet status and affiliation with an academic university) (Woodward & Willegerodt, 2022). Notably, all organizational level interventions identified by this review focused on new graduate registered nurses (NGRNs).
Table 2. Unit-Level and Organizational Level Interventions
| |
Theme |
Reference(s) |
|---|---|---|
| Unit-level Interventions |
Transformational Leadership |
Conroy et al., 2023 |
| Organizational support |
Galanis et al., 2024; Woodward & Willegerodt, 2022 |
|
| Organizational-level Interventions |
Preceptorship programs |
Aparício & Nicholson, 2020 |
| Clinical supervisor programs |
Aparício & Nicholson, 2020 |
|
| Nurse residency programs |
Mohamed & Al-Hmaimat, 2024; Vázquez-Calatayud & Eseverri-Azcoiti, 2023; Woodward & Willegerodt, 2022 |
|
| Adaptive education |
Vázquez-Calatayud & Eseverri-Azcoiti, 2023 |
|
| Individualized mentoring programs |
Vázquez-Calatayud & Eseverri-Azcoiti, 2023 |
|
| Combined residency and meeting |
Vázquez-Calatayud & Eseverri-Azcoiti, 2023 |
|
| Best-fit orientation |
Vázquez-Calatayud & Eseverri-Azcoiti, 2023 |
|
| Organizational support |
Woodward & Filigreed, 2022 |
Unit-Level Interventions (implemented within nursing units and focused on retaining the existing nursing workforce)
Transformational leadership (TL) is a supervisor’s ability to inspire a shared vision, encourage innovation, recognize individual contributions, and create a sense of purpose and belonging within a team to facilitate the accomplishment of work. This leadership style includes four main components: 1) idealized influence (acting as a role model to establish trust and respect), 2) inspirational motivation (enabling staff to achieve organizational and personal goals), 3) intellectual stimulation (encouraging staff to develop new ideas and pursue continuous learning opportunities), and 4) individualized consideration (encouraging staff through support and positive feedback).16 Supervisors demonstrate a transformational leadership style by connecting employee interests with the overall interests of the organization, role-modeling, and supporting employees in the development of strengths. Conroy et al. (2020) conducted a review of twelve studies that assessed the relationship between TL and nurse retention. Eleven of the 12 studies demonstrated a positive correlation between TL and nurse retention in hospital setting. Only 1 study (Abualrub & Alghamidi, 2012) found a statistically insignificant relationship between TL and nurse retention. The review noted further research is necessary to investigate which specific components of the TL style are significantly related to staff retention (Conroy et al., 2020).
Organizational support includes efforts to create a work environment that meets the professional and personal needs of the nurse. Components include employer-specific culture, working conditions, resources, and benefits in place to enable an employee to perform responsibilities efficiently, safely, and which contribute to the professional advancement of the employee. Unit-level examples include adequate staffing and workload flexibility, supervisory support, work schedules that promote healthy work-life balance, resources to protect the safety of the employee, opportunities for continuing education and job advancement, and assistance with managing stressful situations. Perceived organizational support includes a nurse’s overall perceptions and beliefs of how an organization values and respects their contributions, and cares about their well-being and job satisfaction.17 In a review of the association between organizational support and turnover intention of nurses, Galanis et al. (2024) analyzed eight studies which used the Survey of Perceived Organizational Support (N=7) and the Perceived Organizational Support – Simplified Version Scale (N=1) to measure organizational support. Turnover intention was evaluated using the Turnover Intention Scale (N=3), or other validated researcher-developed scales (N=5). All studies showed a negative correlation between organizational support and turnover intention. The pooled correlation coefficient was −0.32 (95% confidence interval: −0.42 to −0.21), a moderate negative correlation showing that as organizational support increases, nurse turnover intention decreases.
Organizational-Level Interventions (organization-wide interventions focused on new graduate nurses)
In their review of six studies of preceptorship and clinical supervision programs, Aparício and Nicholson (2020) found that preceptorship programs and clinical supervision programs have a positive relationship with the NGRN retention rate (Table 2). Preceptorship programs partner an NGRN with an experienced nurse who provides performance evaluations, role-modeling, and support as needed. These programs range in length (12 weeks to 12 months), structure (ex: one day/month or all shifts for six months), and may be included among other components of NGRN residency programs. Retention rates reported in one study within the review found 86% (n=596/693) of NGRNs were retained from high preceptor support (HPS) hospitals compared to 80% (n=545/682) of NGRNs retained from low preceptor support (LPS) hospitals.22 High preceptor support hospitals are hospitals that provide full support for both preceptees and preceptors (preceptees frequently worked with the preceptor, had different preceptors daily, had one-to-one support and shared workloads, and preceptors benefited from having a reduced workload, a smaller number of preceptees, and the opportunity to frequently work with preceptees). Low preceptor support hospitals provided less support than high preceptor support hospitals.22 Clinical supervision programs support NGRNs by providing support through clinical teaching, buddying, and facilitating professional development over a 12-month period. Hussein et al. (2019) conducted a survey of 87 NGRNs toward the end of a clinical supervision program using the Manchester Clinical Supervision Scale (MCSS) and Intention to Stay in a Clinical Specialty survey.23 After controlling for age, workload expectations, and satisfaction with practice environment, nurses with high satisfaction of clinical supervision had nearly 4 times the odds of intending to remain in the critical care unit (AOR: 3.861, 95% CI: 1.320-11.293) while nurses who had high satisfaction with their unit orientation also had almost 4 times the odds of intention to remain in the critical care unit (AOR: 3.629, 95% CI: 1.236-10.659).
Vazquez-Calatayud & Eseverri-Azcoiti (2023) reviewed 9 studies to identify interventions that promote the retention of NGRNs and concluded that 1-year nurse residency and individualized mentoring programs, addressing core competencies (ex: communication, teamwork, clinical leadership, critical thinking, conflict resolution), specific competencies (ex: specific procedures or techniques), and including preceptorship or mentorship significantly decrease the likelihood of nurse turnover.19 These findings are aligned with the review by Woodward and Willeroudt (2022) which found NGRN training programs to improve retention rates of NGRNs within the first few years of practice20 and the review of by Mohamed & Al-Hmaimat (2024) which concluded that NGRN programs have potential to improve retention rates during the initial 12 months of employment, even within long term care settings.18 Programs designed to onboard and retain NGRNs vary in composition. Best-fit orientation for new graduate nurses is a personalized onboarding approach that aligns orientation content, clinical experiences, and support systems with the individual nurse’s background, strengths, learning style, and career goals.24 This strategy aims to improve engagement, confidence, and clinical readiness during early stages of clinical practice. Diversified adaptive education designs instruction of the NGRN based on the skills, needs and learning styles of the NGRN.25 Individualized mentoring programs establish a one-to-one, long-lasting nurturing relationship between a mentor and mentee support the NGRN transition to practice.26 Nurse residency programs are designed to offer NGRNs in-patient orientation with a preceptor and structured education on core competencies necessary for clinical practice.27 Components may include a period of in-patient orientation with core and service-specific competencies, a preceptor, formal mentoring, debriefing, and self-care sessions. Combined residency and meeting points include residency programs with regularly scheduled, structured check-ins or touchpoints between the new nurse and key support figures (e.g., preceptors, mentors, educators, or managers).28,29 These meetings are strategically designed to monitor progress, provide feedback, address concerns, and offer emotional and professional support. Significant improvements in turnover and retention rates were found in two studies that included a combined program as an intervention.28,29 Woodward and Willgeroudt’s (2022) systematic review of 31 articles related to RN turnover and retention in the United States identified organizational-level supports that impact NGRN work outcomes. Specifically, retention rates of NGRNs were greater in hospitals with Magnet accreditation (92%) than non-Magnet accreditation (77%) and hospitals affiliated with a university also had higher retention of NGRNs (88%) than those without university affiliation (82%).30
Table 3. Systematic Review Nurse Work Outcome Findings
| Author(s) |
Published year |
Findings |
|---|---|---|
| Aparício & Nicholson15 | 2020 |
Evidence exists that preceptorship programs and clinical supervision programs may have a positive relationship with nurse retention.
Further analysis of those nurses who indicated an intention to remain in critical care revealed that high satisfaction with clinical supervision and high satisfaction with unit orientation were significant predictors. |
| Conroy et al.16 | 2023 |
Evidence exists that transformational leadership (TL) may have a positive relationship with nurse retention.
Further research is needed to assess which specific components of TL (idealized influence, inspirational motivation, intellectual stimulation, individualized consideration) are significantly related to retention. |
| Galanis et al.17 | 2024 |
As organizational support increases, turnover intention decreases.
The pooled correlation coefficient was −0.32 (95% confidence interval: −0.42 to −0.21). |
| Mohamed & Al-Hmaimat18 | 2024 |
All studies showed nurse residency programs have a positive impact on lowering turnover rates and increasing retention rates.
|
| Vázquez-Calatayud & Eseverri-Azcoiti19 | 2023 |
1-year nurse residency and individualized mentoring programs, addressing core and specific competencies and including preceptorship or mentorship, significantly decrease the likelihood of nurses' turnover rate
Significant improvements in turnover and retention rates were found in two studies that included a combined program as an intervention: the quasi-experimental study with a control and intervention group by Hu et al. (2015) and the quasi-experimental study with a single group by Koneri et al. (2021).28,29 |
| Woodward & Willgerodt20 | 2022 |
Work outcomes are impacted by individual-level, unit-level, and organizational-level factors. Unit-level and organizational-level interventions identified.
Unit Level
Organizational Level
Facilities with established NGRN training programs experience the lowest 1-year turnover rates compared to those with newer programs or no program at all. |
Conclusion
While expanding enrollment and graduates from nursing programs is an important component of increasing the supply of nurses in the NC workforce, findings from NC Nursecast demonstrate that efforts to retain our existing nurse workforce are even more important.10,31,32 This report provided an overview of research that quantitatively assessed interventions to increase nurse retention. Heterogeneity in the interventions implemented and the tools used to measure retention limit our ability to identify best practices. Galanis et al. (2024) had similar findings in their systematic review and noted that rigorous research is still required to identify best practices in retaining nurses. However, the nine overarching intervention themes identified in the literature showed positive impacts on nurse retention and support the NCIOM-recommended interventions for nurse retention in NC. The unit-level interventions identified (transformational leadership and organizational support) are applicable to nurses throughout their career and are focused on strategies that employers could implement to retain nurses. The organizational-level interventions identified in this review (preceptorship programs, clinical supervisor programs nurse residency programs, adaptive education, individualized mentoring programs, combined residency and meeting points, and best-fit orientation, and organizational support) are specifically targeted to NGRNs and could be implemented by collaborations between nursing employers and educators in the state.
References
-
NC Nursecast: A Supply and Demand Model for Nurses in North Carolina. The Program on Health Workforce Research and Policy at the Cecil G Sheps Center. UNC Chapel Hill. Accessed 11/21/2021, 2025. https://ncnursecast.unc.edu/diffusion/ ↩︎
-
New Supply and Demand Data Reveals Pathways to Address Health Care Workforce Shortages in North Carolina. NC Center on the Workforce for Health. https://workforceforhealth.org/news/hta-health-workforce-survey-data ↩︎
-
Auerbach DI, Buerhaus PI, Donelan K, Staiger DO. Projecting the Future Registered Nurse Workforce After the COVID-19 Pandemic. JAMA Health Forum. 2024;5(2):e235389-e235389. doi:10.1001/jamahealthforum.2023.5389 ↩︎
-
Colosi B. 2025 NSI National Health Care Retention & RN Staffing Report. 2025. March 2025. https://www.nsinursingsolutions.com/Documents/Library/NSI_National_Health_Care_Retention_Report.pdf ↩︎
-
Jones CB. Revisiting nurse turnover costs: adjusting for inflation. Journal of Nursing Administration. 38(1)doi:10.1097/01.NNA.0000295636.03216.6f ↩︎
-
Bae SH. Noneconomic and economic impacts of nurse turnover in hospitals: A systematic review. International Nursing Review. 2022;69(3):392-404. ↩︎
-
Lasater KB. Addressing the Nurse Retention Crisis—Leveraging Policies Supported by Evidence. JAMA Network Open. 2024;7(7):e2421635-e2421635. doi:10.1001/jamanetworkopen.2024.21635 ↩︎
-
Muir KJ, Porat-Dahlerbruch J, Nikpour J, Leep-Lazar K, Lasater KB. Top Factors in Nurses Ending Health Care Employment Between 2018 and 2021. JAMA Network Open. 2024;7(4):e244121-e244121. doi:10.1001/jamanetworkopen.2024.4121 ↩︎
-
Galanis P, Moisoglou I, Papathanasiou IV, et al. Association between organizational support and turnover intention in nurses: A systematic review and meta-analysis. MDPI; 291. ↩︎
-
Caroline Spencer AJ, Evan Galloway, Catherine Moore, Erin Fraher. How has RN Retention in North Carolina Changed over Time? 2025. NC Health Workforce: Research Blog. https://nchealthworkforce.unc.edu/blog/rn-retention/ ↩︎
-
The Health Workforce in North Carolina: Challenges and Opportunities, (2024) (Erin Fraher). https://www.shepscenter.unc.edu/wp-content/uploads/2024/02/Legislative-Fellows-January-2024_Shortened-for-Newsletter-002.pdf ↩︎
-
Fifty-Fourth World Health Assembly: Resolutions and Decisions. 2001. May 2001. https://iris.who.int/bitstream/handle/10665/260183/WHA54-2001-REC1-eng.pdf ↩︎
-
Committee on the Robert Wood Johnson Foundation Initiative on the Future of Nursing atIoM. The future of nursing: Leading change, advancing health. National Academies Press; 2011. ↩︎
-
Howard C. 2020 Vision–The Year of the Nurse and Midwife. International Nursing Review. 2019;66(4):453-455. ↩︎
-
Time for Action: Securing A Strong Nursing Workforce for North Carolina. 2024. May 2024. https://nciom.org/wp-content/uploads/2023/09/NCIOM-Nursing-Task-Force_Time-For-Action.pdf ↩︎
-
Aparício C, Nicholson J. Do preceptorship and clinical supervision programmes support the retention of nurses? British Journal of Nursing. 2020;29(20):1192-1197. ↩︎
-
Conroy N, Patton D, Moore Z, O’Connor T, Nugent L, Derwin R. The relationship between transformational leadership and staff nurse retention in hospital settings: A systematic review. Journal of Nursing Management. 2023;2023(1):9577200. ↩︎
-
Mohamed Z, Al-Hmaimat N. The effectiveness of nurse residency programs on new graduate nurses’ retention: Systematic review. Heliyon. 2024;10(5) ↩︎
-
Vázquez‐Calatayud M, Eseverri‐Azcoiti MC. Retention of newly graduated registered nurses in the hospital setting: A systematic review. Journal of Clinical Nursing. 2023;32(19-20):6849-6862. ↩︎
-
Woodward KF, Willgerodt M. A systematic review of registered nurse turnover and retention in the United States. Nursing Outlook. 2022;70(4):664-678. ↩︎
-
Salmond SW, Cadmus E, Black KK, Bohnarczyk N, Hassler L. Long-Term Care Nurse Residency Program: Evaluation of New Nurse Experiences and Lessons Learned. The Journal of Continuing Education in Nursing. Oct 2017 2024-08-07 2017;48(10):474-484. doi:https://doi.org/10.3928/00220124-20170918-09 ↩︎
-
Blegen MA, Spector N, Ulrich BT, Lynn MR, Barnsteiner J, Silvestre J. Preceptor support in hospital transition to practice programs. JONA: The Journal of Nursing Administration. 2015;45(12):642-649. ↩︎
-
Hussein R, Salamonson Y, Hu W, Everett B. Clinical supervision and ward orientation predict new graduate nurses’ intention to work in critical care: Findings from a prospective observational study. Australian Critical Care. 2019;32(5):397-402. doi:10.1016/j.aucc.2018.09.003 ↩︎
-
Torres DA, Jeske L, Marzinski SJ, Oleson R, Hook ML. Best fit orientation: An innovative strategy to onboard newly licensed nurses. Journal for nurses in professional development. 2022;38(6):350-359. ↩︎
-
Chen S-F, Fang Y-W, Wang M-H, Wang T-F. Effects of an adaptive education program on the learning, mental health and work intentions of new graduate nurses. International Journal of Environmental Research and Public Health. 2021;18(11):5891. ↩︎
-
Zhang Y-p, Huang X, Xu S-y, Xu C-j, Feng X-q, Jin J-f. Can a one-on-one mentorship program reduce the turnover rate of new graduate nurses in China? A longitudinal study. Nurse Education in Practice. 2019;40:102616. ↩︎
-
Wolford J, Hampton D, Tharp-Barrie K, Goss C. Establishing a nurse residency program to boost new graduate nurse retention. Nursing management. 2019;50(3):44-49. ↩︎
-
Koneri L, Green A, Gilder RE. Touchpoints: a business strategy to retain new graduate nurses. JONA: The Journal of Nursing Administration. 2021;51(7/8):401-408. ↩︎
-
Hu Y-C, Chen S-R, Chen IH, Shen H-C, Lin Y-K, Chang W-Y. Evaluation of work stress, turnover intention, work experience, and satisfaction with preceptors of new graduate nurses using a 10-minute preceptor model. The Journal of Continuing Education in Nursing. 2015;46(6):261-271. ↩︎
-
Blegen MA, Spector N, Lynn MR, Barnsteiner J, Ulrich BT. Newly licensed RN retention: Hospital and nurse characteristics. JONA: The Journal of Nursing Administration. 2017;47(10):508-514. ↩︎
-
What The Data Say About the Nursing Workforce in North Carolina, (2023) (Taskforce on the Future of the Nursing Workforce). https://nciom.org/wp-content/uploads/2023/02/Fraher_NC-IOM-Nursing-Taskforce-02-28-23.pdf ↩︎
-
Patel E, Fraher E. The Impact of COVID-19 on Nurse Practitioner Turnover in Hospital and Primary Care Settings. June 2025. Panel Presentation. 2025 Annual Research Meeting; ↩︎